Medicine X | Nokia
|
|
A global community of researchers, patients,and technologists. Five teams challenged torethink how research is done. |
Medicine X | Nokia Digital Health Challenge
In 2016, five teams from some of the world’s leading medical research institutes were selected to explore how digital health devices could shape the future of research. Each study was inspired by our Everyone Included™ research principles, which emphasize the role of patients and multidisciplinary care teams in study design.
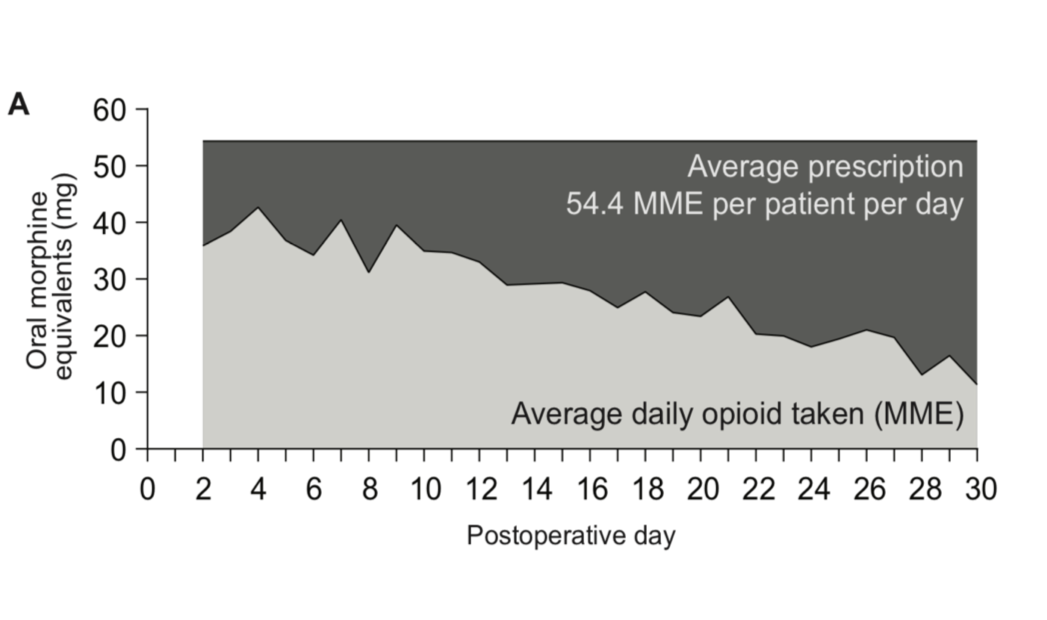
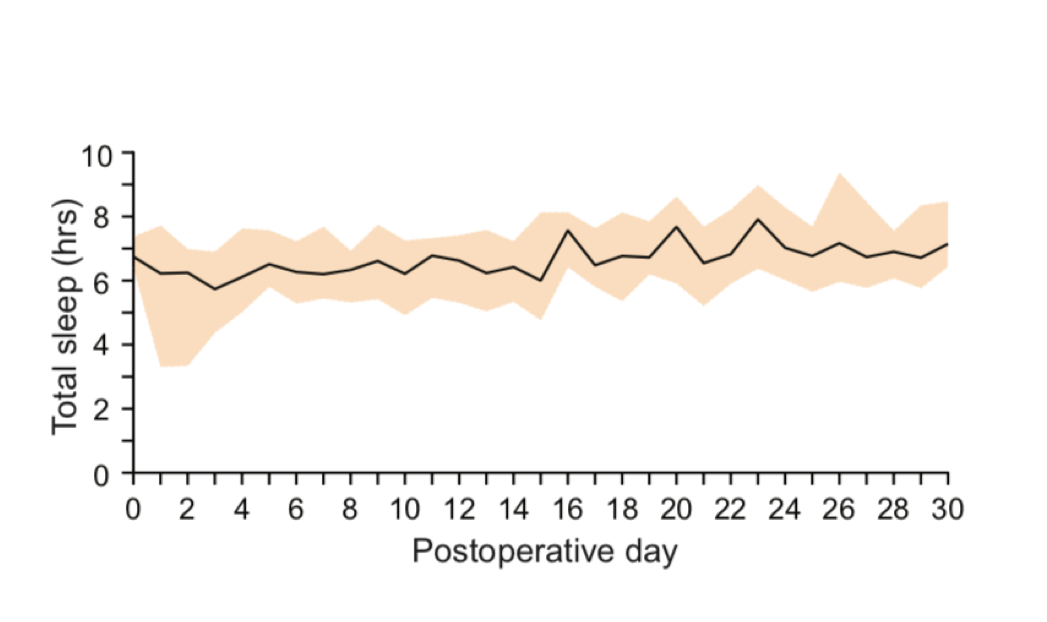
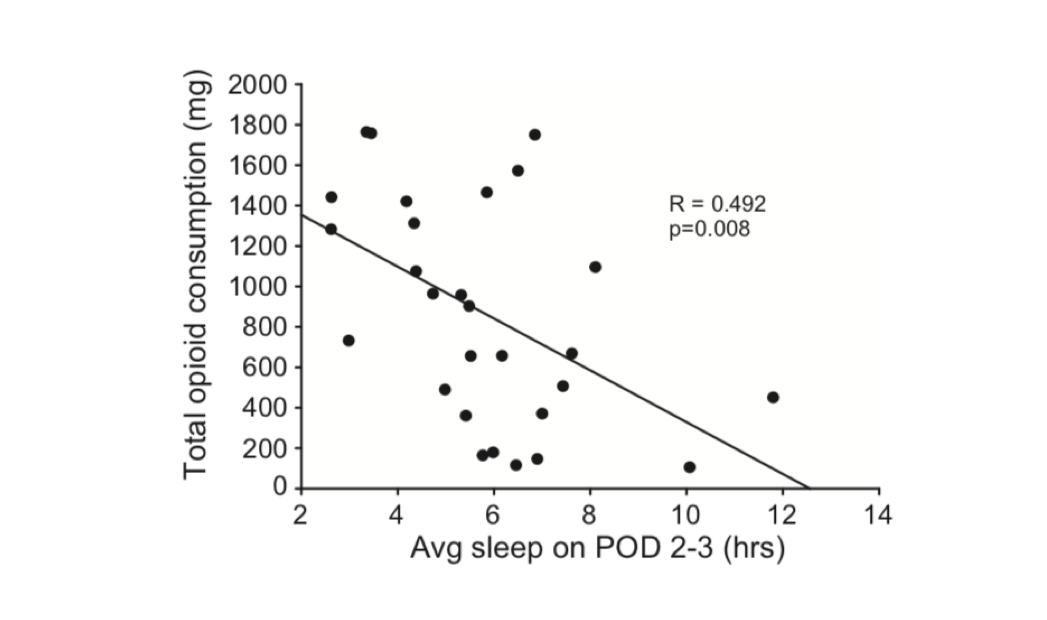
The teams used NOKIA devices, including activity trackers, sleep monitors and smart scales, to investigate a range of clinical problems from heart failure management to opioid use post surgery. These new streams of behavioral data provided unique insights into a part of the patient journey that is often overlooked.
Read below about the five finalist teams and the winning study. This is the new era of Everyone Included research, empowered by the patient and by technology.
“Digital Health is about collaboration. Our Everyone Included™ model allows research teams to co-develop research in digital health”
~Larry Chu, MD, Professor, Stanford Medicine X

“Stanford Medicine X allows us to assess the impact of digital health technology and imagine how it can be included into a more patient-centric care system.”
~Nicolas Schmidt, Nokia/Withings
Physical activity, sleep and cognitive function
Technical University of Denmark
PI: Francois Patou, PhD
Background:
An estimated 18.7% of the general population lives with Mild Cognitive Impairment (MCI) [1], a syndrome characterized by a cognitive decline greater than expected for an individual of a given age and education level, but that does not notably interfere with activities of daily life. Around 38% of MCI cases develop into dementia within 5 years. For older adults, physical activity has been correlated with preserving cognitive functioning as well as promoting better sleep quality. Likewise, studies have shown that sleep disturbances promote cognitive decline and other neuropsychiatric features. Although these associations between physical activity, sleep quality, and cognitive functioning are widely acknowledged, the mechanisms leading to the observed patterns are yet to be determined.
Objective: Leverage Nokia digital health products pervasively night and day to observe associations between and among physical activity, sleep quality, and cognitive function.
Nokia Connected Health in Heart Failure Management
Johns Hopkins
PIs: Michael Yu MD; Seth Martin, MD, MHS; Rosanne Rouf, MD
Background: Over six million Americans are affected by heart failure (HF) and nearly one million new cases are diagnosed annually. Despite advances in care, mortality at five years is nearly 50%, surpassing many cancers. The cornerstone of HF management is close follow-up with providers, rapid medication titration to achieve optimal dosing guided by blood pressure (BP) and heart rate, and adherence to significant lifestyle changes. In patients with the most severe class of HF, limiting sodium and fluid intake and daily monitoring of weight become central aspects of symptom management. As the vast majority of management occurs at home, connected health has emerged as a technology that may enable patients to engage in more proactive disease self-management. However, there has not yet been a study that investigates its potential benefit in patients with HF.
Objective: To assess whether connected health technology improves engagement and lifestyle activation in the medically complex and resource intensive HF population.
Measuring sleep in very early onset psychosis using the Withings Aura
Boston Children’s Hospital
PI: Catherine Brownstein, MPH, PhD
Background: Schizophrenia is a devastating mental disorder that affects 1% of the world’s population and often leads a deteriorating course with premature mortality. Sleep disturbances are often seen in schizophrenia patients, with 80% of hospitalized individuals with schizophrenia having some form of sleep disorder. The most commonly seen disorder is obstructive sleep apnea, which is a risk factor for sudden cardiac death in schizophrenia.
Boston Children’s Hospital (BCH) has amassed a cohort of children with very early onset psychosis (VEOP, defined as onset before age 13). As this rare but devastating condition is related to adult-onset schizophrenia, we hypothesized that sleep disorders are also occurring in this population. Severe patients often miss appointments due to inability to travel, so employing patient-reported data is ideal for those with this condition.
Objective: Aim 1 was to analyze sleep/wake cycles between children with very early onset psychosis for signs of a sleep disorder. Aim 2 was to investigate changes in sleep patterns due to parental awareness of problems highlighted by the Withings Aura. Correcting childhood sleep disorders in this vulnerable population may lead to improved outcomes later in life.
Use of Personal Data in Predicting and Preventing Postpartum Depression
PI: Simal Ozen Irmak, PhD
Background: One in nine new mothers experiences postpartum depression (PPD), a common and often under-diagnosed condition that hinders the health and wellbeing of the whole family and costs over $1 billion to society.
Although certain risk factors are known, there are not any comprehensive tools integrated into the maternal care practice, to monitor the health of the mother and to predict the development of PPD and to offer timely interventions. Hence, despite its high occurrence, little is known about the development of PPD; and even less is done for prevention or for timely-diagnosis.
Objectives: Track personal health and wellness metrics, such as sleep, activity, and mood, for 3 months postpartum to develop a framework 1) to predict the women at risk of developing PPD, and 2) to improve the postpartum experience.